Is there any Scientific Basis for Chiropractic?
Anatomy and Physiology as it relates to chiropractic paradigm
I have written this section for my patients who over the past 30 years have wanted to understand how chiropractic care works. I have been very fortunate to have a diverse patient base, including teenagers, manual labors to college professors and other healthcare providers. All people who wanted to understand the science behind the chiropractic paradigm. To do this, it is necessary to understand that most of the information that now is understood about anatomy and physiology has been updated and revised by current research. Much that I am relating has been published in many different forums from research to clinical observation. I know that some think or believe that most health care interventions are as well grounded in science as what I am presenting in these notes. Remarkably, less than 25% by some conservative estimates of what is currently used routinely in healthcare has double blind studies to substantiate the intervention.
The information below is from generally available references and links that can be found in the library or on the web. There are extensive textbooks and articles on these topics available, but these are usually only found in the bookstores and libraries of chiropractic colleges. (Not a lot of students, other than chiropractic students study the different names of all the joints and articulations involved in the spine or have an interest in the names for each of them.)
Even The Department of Veterans Affairs has added a chiropractic residency program.
So here is the science of today!
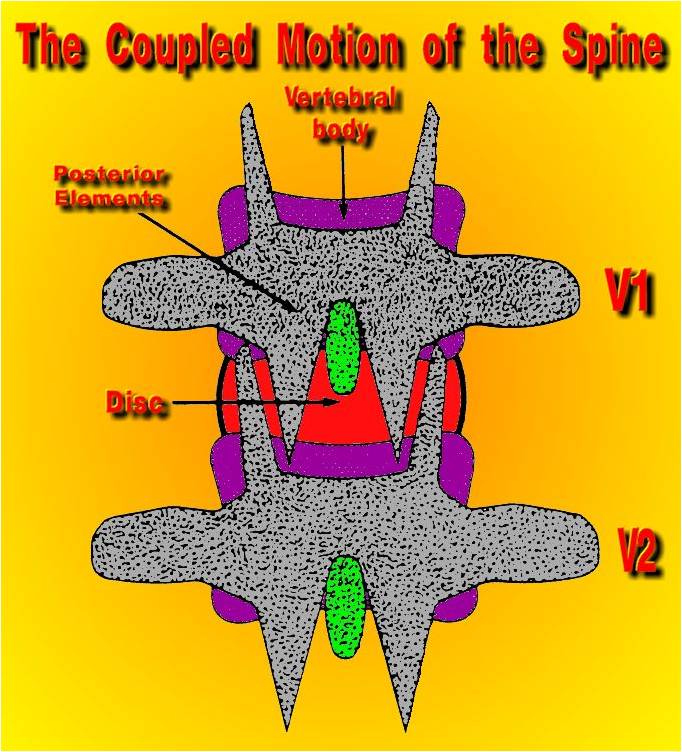
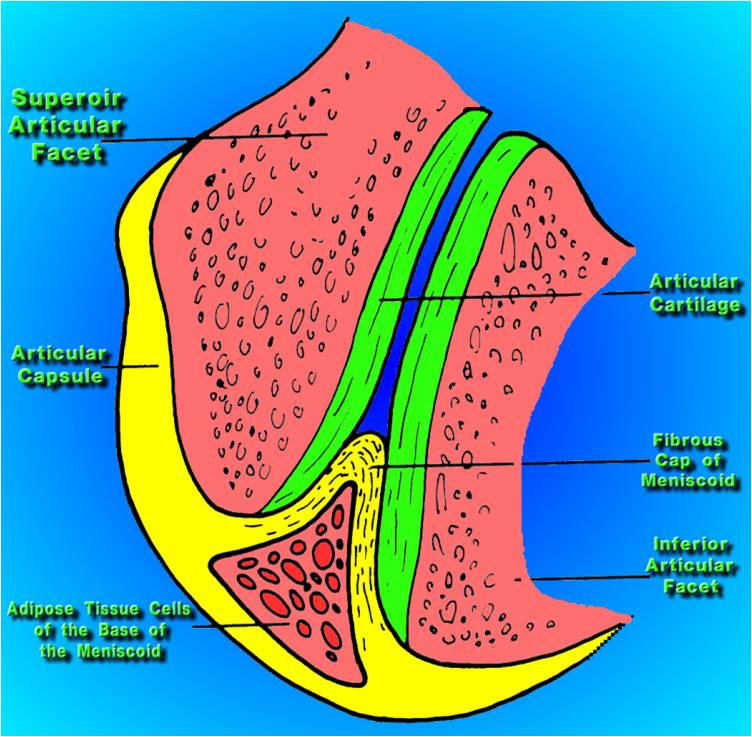
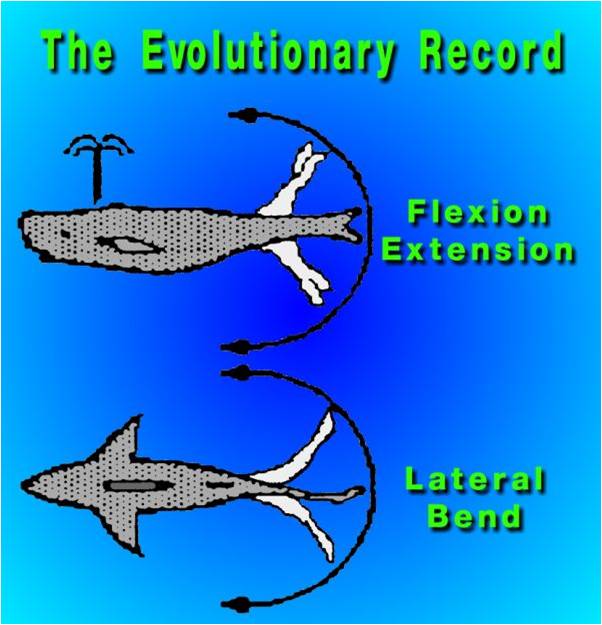
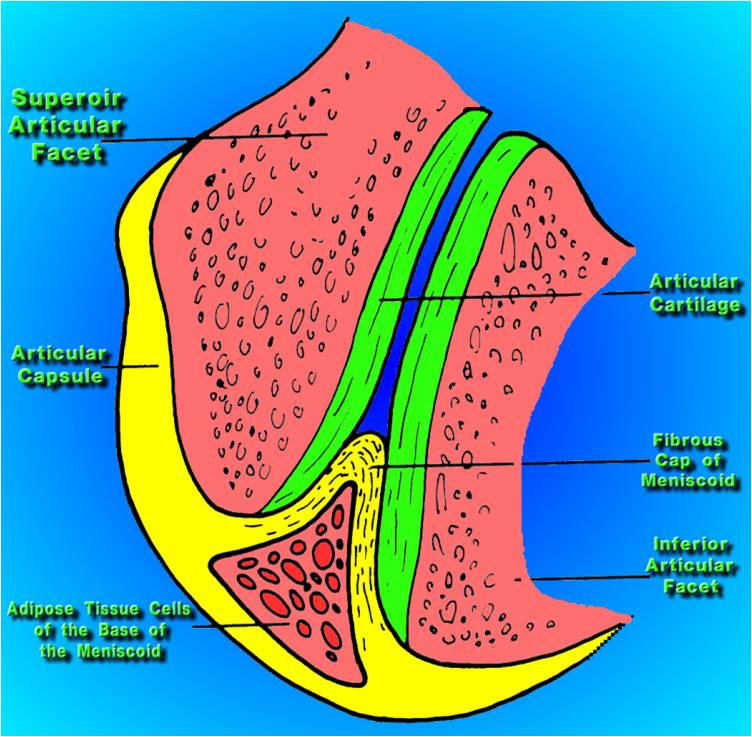
The two joints on the back surface of vertebrae are called a facet or zygapophseal joint.
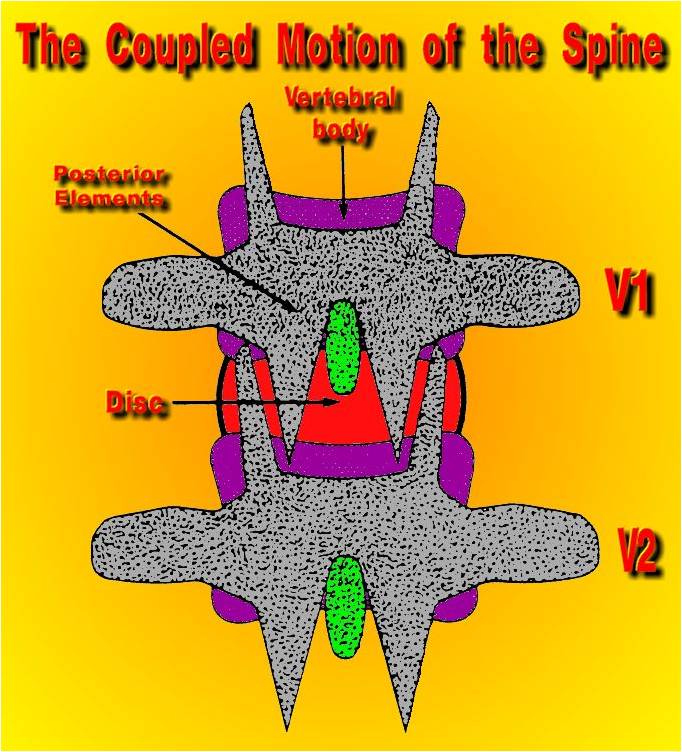
(Back View of the spine-typical)
These joints (facet or zygapophseal) are the ones which are involved in guiding stability of the back and were believed to have a passive role in back activity such as walking and almost everything else.
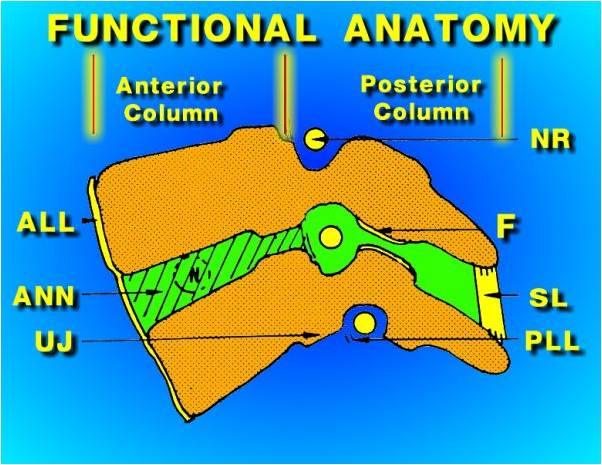
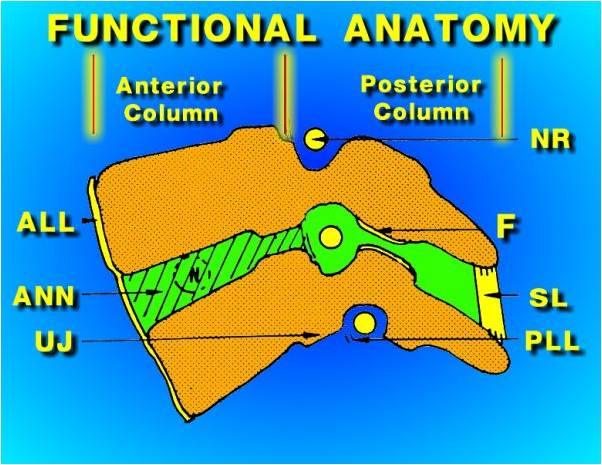
(Side View of spine-typical)
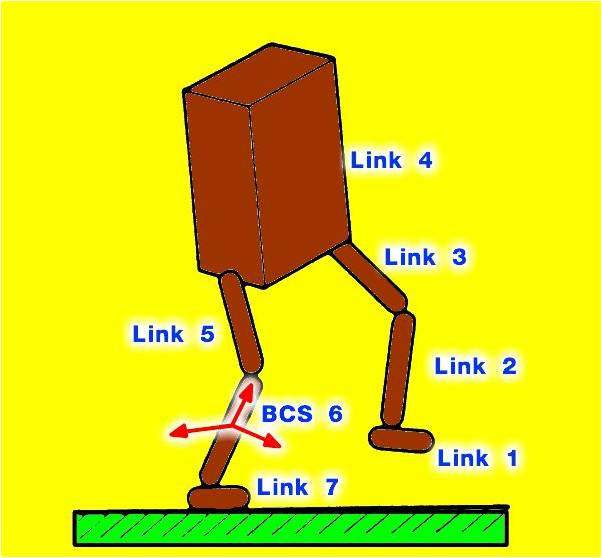
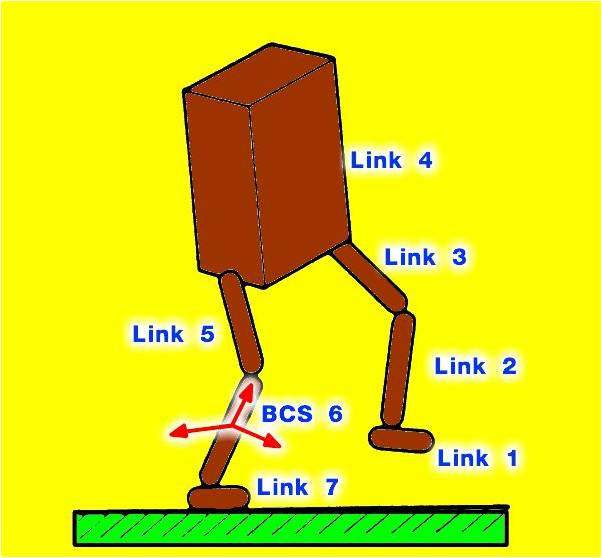
This is one of the earlier models of how the back worked and it is called "The Box Theory".
The problem with this model is that the energy expenditure of walking was possible, but the energy of running did not make fit this model.
The world's fastest runner would have to look like this person, if the model was accurate.
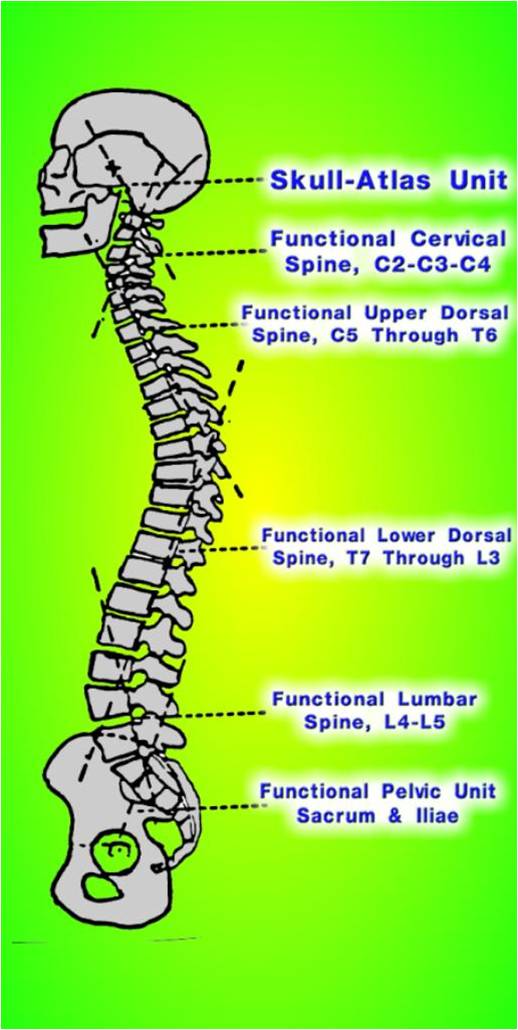
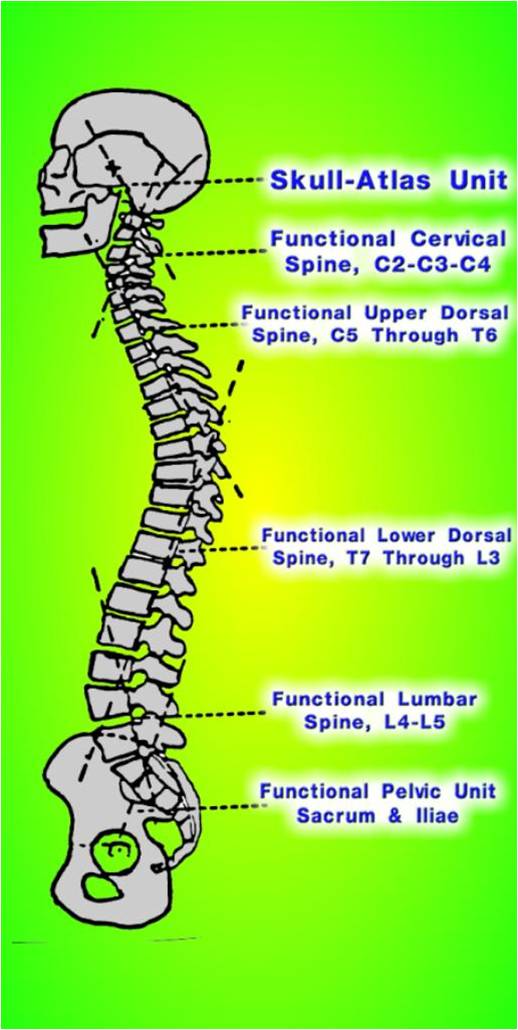
This is a part of one of the model's that is used currently to describe the back during a static posture position. (Harrison Model)
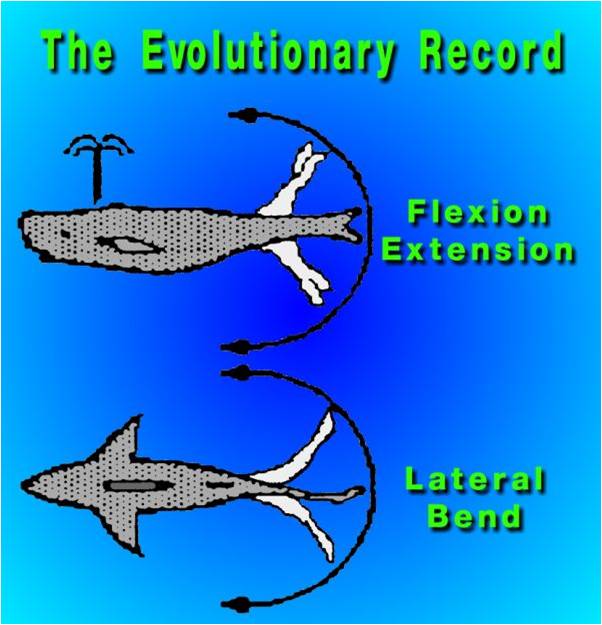
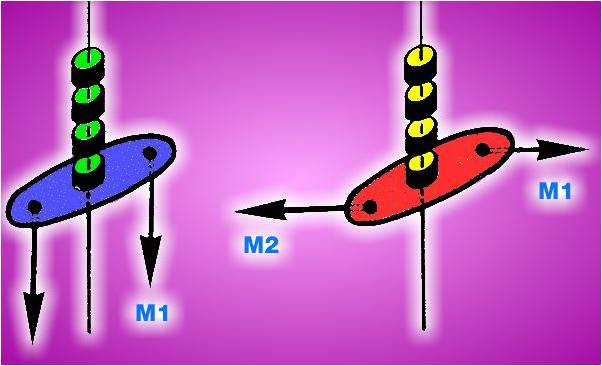
When you start looking at an animated movement model, the best current model is the “spinal engine model” developed by a physicist Serge Gracovetsky PhD. He was not trained to “know” how the back functioned so, from his paradigm as a physicist, he looked at bipedal gate from an evolutionary prospective. His theory states that bipedal gate cycle are an adaptation of the flexion-extension movements of whale and the left and right lateral movements of a shark.
Not intentionally, Gracovetsky has provided an evolutionary model that follows parsimony in describing the development of bipedal gate. And lays the skeletal (anatomical framework) to describe joint movements that responds to chiropractic care. Not everybody is happy about this and sadly the detractors are not aware of the other important research that gives teeth to this theory.
The joint capsular ligament, with its innervation forms a receptor field ( my hypothesis or assertion). The capsular (facet-zygapophseal) receptor fields also have impact on secondary location distant to the facet-zygapophseal joint. The chiropractic term for the neurological aspect of this effect was originally subluxation. Then the term subluxation complex was added to better describe the different aspects (vascular, neurological, lymphatic, skeletal, etc.) Later the term, for the neurological aspect, was updated to Dysafferentation.

It has a primary effect on the Multifidus muscles of the spine. Joint fixation,
induces atrophy and fatty infiltration of these muscles. The disuse of the spinal muscles produce sarcopenia.
Upton Sinclair quotes "It is difficult to get a man to understand something, when his salary depends on his not understanding it."
The typical human spine has 48 joints called facet or zygapophseal joints. Here is the start of some of the more traditional medical doctors explanation of the spine.
The medical description of this phenomenon was described in "The Human Spine in Health and Disease" by Georg Schmorl (5th German edition by Herbert Junghanns). The description was more of a staging of the process of subluxation than an anatomy and physiology description.
The initial localized problem was called an Inefficient Motor Segment (Intervertebral Insufficiency) Definition
Group 1 - Changes and complaints in the immediate vicinity of the disturbed motor segment.
Group 2- Symptoms which are conducted through neural and vascular pathways and which also have been termed as symptoms (spondylogenic) of syndromes of spinal cause.
Group 3- Spondylogenic disease which have become independent and have developed originally from the second group.
The neuroanatomy of the facet or zygapophseal joint was first partially described as the note that there was a nerve that innervated the joint capsule recurrent meningeal nerve or the recurrent nerve of Von Luschka.
This evolved into the frame work of describing a complete classification of the nerve ending (receptor types) that innervate the joint capsule of the (facet or zygapophseal) joint.
Today, the neurological parts of these joints take on a totally different importance; not, just it's a chiropractor invented term "subluxation" to be dismiss. The claims of several detractor of chiropractic, is that it has no basis in scientific writings. The follow information may lead the cause of the honest intelligent scientist to re-examine that position.
Articular neurology is the classification system devised by BD Wyke.
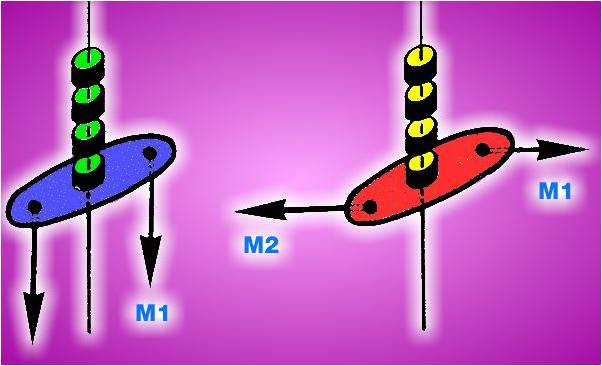
The next major step is to understand that the joint capsule is a (primary and rudimentary) receptor field and what the implications of that realization means. To begin with a background of receptor field processes is needed to follow the importance. The idea that we have five senses and the receptor fields are separate and distinct is one of those learned scientific truths that may more accurately describe a built in scotoma (blind spot). The first example that seeing is only with the eyes was challenged with the skin as a surrogate eye study. Then further studies produced this paper “the all seeing tongue-taste the light”. Exploiting the idea to vision from the tongue has produced Brain Port for vision and after my own heart, balance training with a much larger understanding of the implications of these ideas. Then the idea that the complexities of the nervous system connection, to which the eyes did not need to be in a complex organism. Box jelly fish. Another interesting aspect of the jelly fish species is the movement patterns of complex behavior tied into each of the 24 eyes.
The next idea was what happens if the facet joint receptor field is disconnected from the upper brain. The U Tube of the chicken without a head as seen on Believe it or not. Realizing, that we now know, that the spinal cord and cerebellum (rethinking the lesser brain) play a critical part of complex behavior patterns; it requires a major shift in our thinking as to how information is obtained and integrated into our body. Paul Bach-y-Rita concept of Neuroplasticity has altered the reality of understanding how the brain functions. As this U-Tube video from the BBC shows .
The ability to condition (Pavlov) internal organs all that is required is a receptor field which can be an interconnected to another receptor field. (Cerebral cortex internal organs) (This book is available in many university libraries.) Then the idea that the Psychoneuroimmunology is a real field of study makes one begin to consider the possible mechanisms how some of the remarkable occurrences that have been purported to be noted with spinal adjustments.
The typical human spine has 48 joints called facet or zygapophseal joints. The above information can be simple state as the following: The capsular ligament(s) when viewed with an electron microscope reveals the existence of receptors. These receptors classified by Dr B Wyke MD as articular receptors (three different types receptors are in the capsular ligament of spinal facet joints). These rudimentary receptor fields display the same properties, as most receptor fields, and can be conditioned aka Pavlov, convey information to the spinal cord and cerebellum (aka Sc Am. Rethinking the Lesser Brain). Several different mechanisms can influence the function of these receptor fields to generate spasm, splinting and/or pain. Then the TM Joints (jaw joints) also have receptors (forming a receptor field) which can produce significant problems for patients (most dentists and Otolaryngologists (ear, noise & throat specialist) have seen patients with this problem). If you are a researcher, make sure to read the full PDF of this article, to understand the impact of the joint receptor fields on the muscles involved in mandible function. I am certain that joint function follow parsimony in biology and this is representative of most joint capsule function. This is my current working model and I am providing this information for clarity.
Here is a recent addition of information on Articular Neurology and Manipulative Therapy from Donald E. Ingber MD, PhD, at Harvard Medical School
One explanation of how manual therapy works is provided by Donald E. Ingber MD, PhD, at Harvard Medical School (2008) who argues for the “concept of cellular mechanotransduction, the process by which cells sense mechanical forces and transduce them into changes in intracellular biochemistry and gene expression.” Based on a prolific, federally funded research program over a number of years, Dr. Ingber has been studying cells on the nanometer scale. He views “the cytoskeleton as an architectural structure that actively generates tensile forces and distributes them to other components inside the cell”. Ingber (2006) suggests that in the living body “the process of cellular mechanotranduction might be more a phenomena of structural hierarchies and biological architecture than the action of any single mechanotransduction molecule”. This has significant implications for the field of manual therapy. Ingber (2006) states that to “seek out and study individual biological parts in isolation without considering contributions of multiscale architecture and invisible internal forces means we will never be able to fully understand how physical forces influence biological form and function.”
The cellular/tensegrity research of Ingeber (2008), connective tissue research of Langevin et al. (2001 and 2002), and the fascial research of Schleip (2003) are critical in our understanding of connective tissue and its applications in the manual therapies.
Wyke’s mechanoreceptor research (1980) has been instrumental in understanding the effects of the manual therapies and in particular joint mobilization/manipulation. Schleip (2003) explains the importance of fascial mechanoreceptors, and with manual manipulation changes can occur in the viscosity of the ground substance and a lowering of sympathetic tonus. Schleip (2003) has also found smooth muscle cells in fascia that appear to be involved in active fascial contractility and have only been reported in large fascial sheets. Pacinian corpuscles are also found in the peritoneum (Stilwell in Schleip 2003 page 15) and can be influenced by manual therapy (Schleip 2003}. Mechanoreceptors have been found in the visceral ligaments (Schleip, 2003). The “belly (enteric) brain” (Gershon in Schleip 2003 p. 17) contains more than 100 million neurons. Many of these sensory neurons function as mechanoreceptors.
Ingber, D.E. (2008) Tensegrity-Based Mechanosensing from Macro to Micro. Progress Biophysics Molecular Biology 97(2-3) pages 163-179
Langevin, H., Churchill, D. Cipolla, M (2001) Mechanical Signaling Through Connective Tissue: A Mechanism for the Therapeutic Effect of Acupuncture. Federation of American Societies for Experimental Biology volume 15 , 2275-2281
Langevin, H., Yandow, J., (2002) Relationship of Acupuncture Points and Meridians to Connective Tissue Planes. The Anatomical Record, 269(6) pages 257-265
Wyke, BD. (1980) Articular Neurology and Manipulative Therapy. In Aspects of Manipulative Therapy. Ed. Idezak, R.M. Lincoln Institute of Health Sciences.
Mechanobiology, Injury and healing: When genetic expression are uniting in mRNA expression as
a result of specific adaptation to imposed demands (SAID).
Well, as long as we are considering the information above, we might also get to this statement:
Next I will go to the spine and discuss the muscular issues:
How “Good” are the outcomes for low back pain with chiropractic care?
Low back care by DC is cheapest with cost for value. You will have to buy the full article to see the details, but the short version is chiropractors can help with back pain and do it for less!
How much does initiating care with a DC vs. MD cost?
The J of American of Family Medicine in 2009 warned membership about Lower Back pain, cost, and Pain medication !
What does it cost with integrative care involving a chiropractic internist, medical physician, and internal medicine work as a team?
How safe is chiropractic and medical care for back problems?
“Failed back surgery syndrome" is a common problem with enormous costs to patients, insurers, and society. The etiology of failed back surgery can be poor patient selection, incorrect diagnosis, suboptimal selection of surgery, poor technique, failure to achieve surgical goals, and/or recurrent pathology.”
|